Quality Pays: How to Increase Your Revenue from the Quality Payment Program
The Centers for Medicare and Medicaid (CMS) stated mission is to promote high quality, affordable, person-centered care. As a result,…
The Centers for Medicare and Medicaid (CMS) stated mission is to promote high quality, affordable, person-centered care. As a result, the CMS clinician payment system has been evolving in recent years to incentivize quality and penalize its absence. This means that practitioners who want to improve their bottom line should look for ways to improve their practice standards in the eyes of CMS.
What is the Quality Payment Program (QPP)?
CMS introduced the Quality Payment Program (QPP) with the passage of the Medicare Access and CHIP Reauthorization Act of 2015. You might know this as MACRA.
The core objects of the QPP are:
- Improving the care beneficiaries receive
- Reducing Medicare costs
- Advancing the sharing of health information between providers and patients
- Educating and empowering patients as active participants in their care
QPP allows the CMS to pay out more money to practitioners who maintain high standards of care as compared to those who provide substandard care.
It literally pays for practitioners to find ways to increase quality of care and performance for Medicare/Medicaid patients.
How Does Payment Work With QPP?
Participation in the QPP is available in two forms: Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM).
Providers may earn (or lose) performance-based payments for the services they provide to Medicare patients through MIPS or APM. While both systems operate on the same principles, the APM approach is more customized, offering incentives to clinicians who provide care in certain focus areas, such as specific clinical conditions or to certain populations.
Performance evaluations assess and assign a score to practitioners based on four factors: quality, cost of care, e-health recording, and improvements in clinical care processes. This score determines whether a practitioner exceeds, meets, or does not meet CMS quality of care criteria and ultimately determines payment.
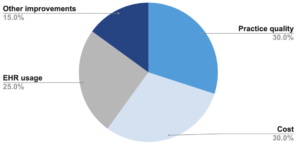
The weighting of these four factors in determining a practitioner score for MIPS is as follows:
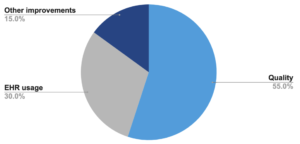
APP does not consider cost, so a practitioner’s score is based on:
How does the QPP impact practitioners?
In a nutshell, quality pays! CMS has stated that its priority is to “Increase the number of beneficiaries in a care relationship with accountability for quality and the total cost of care.” The MIPS and APM performance scores reflect this focus on quality. Practitioners and patients alike benefit from investing in processes and systems that help deliver high-quality care.
How can having connectivity help increase CMS payments?
As part of the QPP practices can earn additional cash based on the value of services they provide, with additional benefits for new care models that improve quality and efficiency.
Relaymed, in combination with your existing point of care instruments, can help you increase the value of your care services in two ways:
- Improve your quality of testing: Most point of care device users currently manually enter test results, which can take up to 10 minutes per test. Using Relaymed you are able to eliminate the time it takes to manually enter results and give that time back to staff to use for patient care and value add services.
- Expand the types of testing that you offer patients: Practices may be hesitant to offer more types of testing due to the complexity that might be involved. Relaymed makes it easy to get results from the device to the EHR. No matter what results are coming through your devices, they will be sent automatically through the Relaymed cloud to the EHR without any manual intervention. Testing can be scaled very easily.
An affordable step towards improving quality and performance
The future of CMS payments and its incentives for providers will be based on improving quality of care, healthcare information integration, and other demonstrated improvements in your clinic that enhance care and reduce costs. You can implement Relaymed to increase efficiencies in your practice while improving your QPP score and subsequent CMS payments.
Interested in learning more about how you can get your CMS bonus?
